Being productive is hard.
Most of us aren’t any good at it naturally. In fact, recent reports suggest we’re only productive for about 3 hours in a normal 8-hour workday.
That means in a 40-hour work-week only 15 hours are spent productively.
If you’re studying for multiple exams or trying to meet a tight deadline at work on top of all the other responsibilities you have in your life — you’re going to need to get more than 3 productive hours out of your day.
Modafinil offers a unique solution to this problem.
It’s classified as a stimulant and eugeroic — which means it keeps us awake and helps us focus on the task at hand.
Modafinil is an extremely useful tool for forcing us into a productive mental state for several hours at a time.
For its 12-18 hour duration, it can turn us into an absolute machine.
We focus intently on our work, become immune to distractions, and remain awake and alert for several hours longer than the average workday provides.
Here, we’ll go over the best ways to get modafinil online and review the most popular vendors in this space.

First Of All, Why Buy Modafinil Online?
Modafinil is a prescription medication, used for treating ADD/ADHD, and narcolepsy. Unlike other medications in its class, it’s not an amphetamine, and therefore lacks many of the negative side effects associated with amphetamine use.
Modafinil is a popular cognitive performance-enhancing medication. Students, entrepreneurs, business owners, and creatives can all benefit from using modafinil to boost productivity.
In most parts of the world, modafinil requires a prescription to purchase.
This means that you can only buy modafinil at pharmacies, which usually sell the brand-name version of the drug, Provigil®.
These brand-name versions can be very pricey, costing customers $300-$1200 per month for a prescription.
Generic versions of the drug offer identical chemicals, at a fraction of the cost.
People with a doctor’s prescription for these medications often choose to buy them online in order to cut this cost down dramatically. The cost of a month’s supply of Modalert, for example, is between $10 and $20.
Most of the online sources for modafinil are selling the generic versions of modafinil and its sister compound, armodafinil.
What Generic Versions Are Available?
The manufacturer of brand name modafinil (Provigil) is the US-based Cephalon Inc.
Generic versions include ModaXL by HOF (a new brand with the purest modafinil formula), Modavinil by Centurion Remedies, Modalert by Sun Pharmaceuticals, and Modvigil by Hab Pharmaceuticals.
There are also four armodafinil generics, including ArmodaXL by HOF (a new brand with the purest armodafinil formula), Armodavinil by Centurion, Waklert by Sun Pharmaceuticals, and Artvigil by HAB Pharmaceuticals.
All of these medications are nearly identical, but the generic versions are sold at a much lower cost.
- Modalert 200mg
- Modvigil 200mg
- Waklert 150mg
- Artvigil 150mg
-
Modalert 200mg
-
Company
-
Core Ingredient
Modafinil
-
Price from
$0.53 in 7 days
-
Dosage
Between
50 – 200 mg per day -
Coupons
Pay with crypto -20%ENJOYMXL10 for -10%
-
Good for
-
Alertness
-
Mental Focus
-
Agility
-
Energy
-
Motivation
-
-
Effect hours
-
Onset 1 hr.
-
Peak 6 hr.
-
Drop 2 hr.
- Buy Now
-
Modvigil 200mg
-
Company
-
Core Ingredient
Modafinil
-
Price from
$0.39 in 7 days >
-
Dosage
Between
50 – 200 mg per day -
Coupons
Pay with crypto -20%ENJOYMXL10 for -10%
-
Good for
-
Alertness
-
Agility
-
Energy
-
Cognition
-
Motivation
-
-
Effect hours
-
Onset 2 hr.
-
Peak 5 hr.
-
Drop 3 hr.
- Buy Now
-
Waklert 150mg
-
Company
-
Core Ingredient
Armodafinil1
-
Price from
$0.59 in 7 days >
-
Dosage
Between
50 – 150 mg per day -
Coupons
Pay with crypto -20%ENJOYMXL10 for -10%
-
Good for
-
Mental Focus
-
Agility
-
Energy
-
Cognition
-
Motivation
-
-
Effect hours
-
Onset 3 hr.
-
Peak 8 hr.
-
Drop 1 hr.
- Buy Now
-
Artvigil 150mg
-
Company
-
Core Ingredient
Armodafinil
-
Price from
$0.41 in 7 days >
-
Dosage
Between
50 – 150 mg per day -
Coupons
Pay with crypto -20%ENJOYMXL10 for -10%
-
Good for
-
Mental Focus
-
Agility
-
Cognition
-
Motivation
-
-
Effect hours
-
Onset 2 hr.
-
Peak 6 hr.
-
Drop 2 hr.
- Buy Now
Rating Criteria
It can be really difficult to find a good modafinil vendor — trust me, I’ve tried a lot of different vendors, and most of the time I was quite underwhelmed.
This is why I started documenting and reviewing vendors for my own use. Here, I’ll outline my top three, and discuss exactly why they stand out above the rest of the crowd.
Let’s go over how I rated each section.
A) Customer Service
One of the main problems I’ve found is that customer service in this industry is sub-par to other industry standards.
Most times, there are no problems with the order, however, in some cases, there’s a problem at the border, or the package doesn’t arrive on time. In the event that a problem arises, it’s crucial that we can contact the company by sending the package to work out a solution.
This was a major factor in determining the quality of each vendor.
B) Price/Value
The next section investigates the price of the products. There are too many online vendors selling their modafinil at higher prices than average, but not offering any added value for this price hike. Others are selling modafinil at a discount, however, the products delivered are either expired, inactive, or short on a couple of pills.
This is unacceptable, so I decided to include the price/value each company has to offer.
A low rating here indicates a poor value for the money while a 5/5 rating indicates excellent value.
C) Discounts
One of the biggest costs a modafinil vendor has is credit card processing fees. This is because most of the international credit card processors charge significantly higher rates to pharmaceutical vendors. This is due to the high risk of chargebacks and returns in the industry.
There’s a simple solution for this — payment with cryptocurrencies like Bitcoin or Ethereum. These forms of electronic money don’t require a bank or payment processor to work and send instant, low-fee transactions across borders.
When paying with Bitcoin, the modafinil vendor will save a large portion of the sale by not having to go through the credit card processor. Some modafinil vendors will transfer these savings to the customer while others keep the difference as profit.
Some vendors will offer other discounts as well to reward returning customers, or through a refer a friend program.
A 5/5 rating in this section would involve a 20% discount when paying with cryptocurrency or other discount options. This is considered the gold standard for the industry.
D) Customer Reviews
People are always reviewing the products they buy, you just need to know where to look.
In the modafinil space, there’s a large number of people talking about their experiences on forums like Reddit or Longecity forums. I’ve taken the liberty to scan through these forums to get a general consensus on a particular vendor to summarise how they’re perceived by the overall community of modafinil users.
A 5/5 rating means the vendor has little to no bad reviews and plenty of raving 5-star reviews among their user base.
E) Product Range
This section highlights the diversity of the products carried. Some modafinil vendors will offer other related products like Piracetam or other nootropics, and others will have only one or two products.
A 5/5 rating includes any company that includes the standard six modafinil products (ModaXL, Modalert, Modvigil, ArmodaXL, Waklert, and Artvigil) — plus at least one other product such as sublingual Modafil MD.
F) User Experience
This section reviews how straightforward the vendor’s user experience is. How easy is it to get to the website, find the products you want, opt-in or out of any discounts, and follow through with payments.
Some of the vendors in this space use complicated and difficult to navigate product pages, slow payment processing, or use spammy sales tactics like popups or email inbox spamming.
A 5/5 rating for this section means the vendor website is simple and easy to navigate, and the payment portal is secure and offers multiple forms of payment including credit cards.
Summary of Rating Criteria for Modafinil Vendors
| 1/5 | 2/5 | 3/5 | 4/5 | 5/5 | |
| Customer Service |
Customer service reps did not answer email or phone call despite multiple attempts. | Customer service response was slow and unhelpful. |
Customer service response was delayed, and offered some problem-solving support. |
Customer service reps were fast and effective at solving any problems with the order. |
Customer service responded within 24 hours and went above and beyond to help with any issues or complaints. |
| Price/Value |
The cost per tablet is well above the average price per pill. Extremely poor value for products delivered. |
Price per pill is average. No additional cost-savings available. Low value. |
Price per pill is average, but vendor offers additional cost-savings such as free shipping or discount options. Average value. | Price per pill is below average, but no additional cost-savings are included. Above average value. |
Cost is below average pricing, and discounts or additional cost-savings are available. High value. |
| Discounts | No discount offered. |
Discounts of less than 5% available. |
Discounts between 10% and 15% available. |
Discounts between 10% and 20% available. |
Discounts of more than 20% are available. |
| Customer Reviews | The vendor has numerous poor reviews by past customers. Poor customer loyalty. |
No customer reviews posted online. |
The vendor has an even mix of good reviews and bad reviews online. Average customer loyalty. |
The vendor has mostly good reviews by past customers, but some bad reviews. Above average customer loyalty. |
The vendor has an overwhelmingly positive review history and excellent customer loyalty. |
| Product Range |
Only one product available. |
Two modafinil products available. |
Three modafinil products available. |
All six standard generic modafinil products available. |
All six standard generic modafinil products available plus other related products. |
| User Experience |
The website is hard to navigate, and payment options are confusing or spammy. |
Website or payment options are confusing. No credit card payment option. |
Website or payment options are confusing. Offers credit card payment option. |
The website is easily navigated and payment portals are fast and efficient. No credit card payment option. |
The website is easily navigated and payment portals are fast and efficient. Offers credit card payment option. |
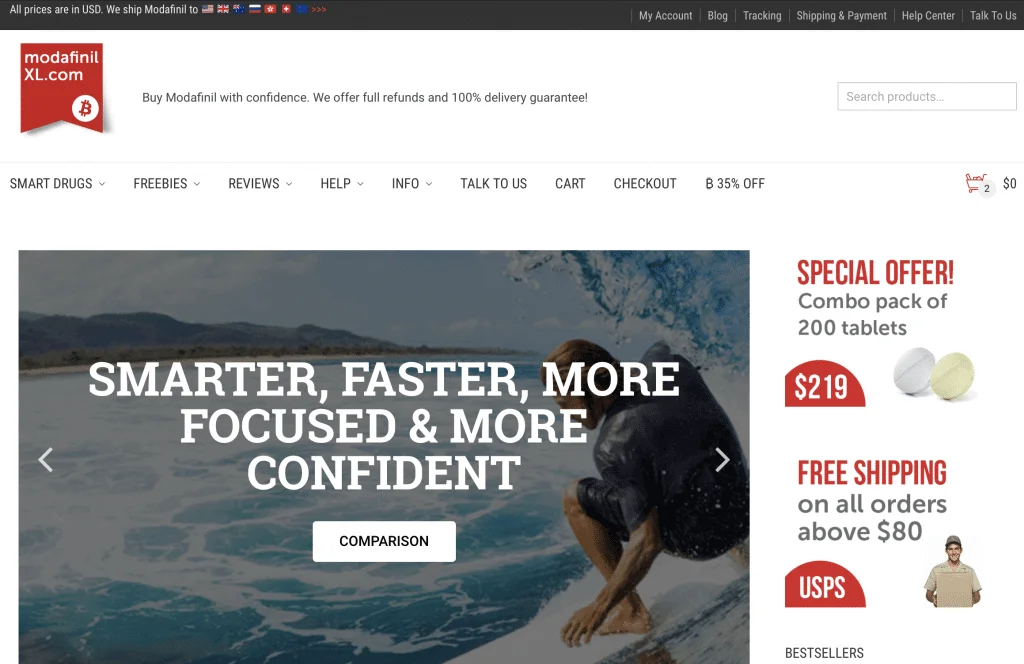
1. ModafinilXL
When Afinil Express, DuckDose, BuyModa.com, and ModafinilCat closed their shops, the modafinil community was at a huge loss.
These were the most popular sources for modafinil around. It had incredibly strong customer loyalty and worked hard to pave the way in the rest of the modafinil space.
There were only three alternatives that ModafinilCat recommended to their loyal customer base; ModafinilXL, Afinil Express, and DuckDose ( UPDATE: both Afinil Express and DuckDose have since closed down too).
A recommendation from ModafinilCat is huge. A company that placed customer satisfaction so highly wouldn’t recommend anything but the best to their loyal customer base — even in closing.
This recommendation from ModafinilCat to its loyal customers says a lot about the reputation ModafinilXL has earned for themselves. A recommendation from Afinil Express is BuyModafinilOnline if you live in the EU.
Placing Order on ModafinilXL Video Tutorial
In this short video, we’re going to go over modafinil purchasing online, a Coinbase account verification. It will help you to get 20% off your purchase on ModafinilXL.
ModafinilXL Review Summary
| Overall Rating | Details | 4.5/5 |
| Price Point | Low-cost online pharmacy with very affordable pricing. Both Modafinil and Armodafinil cost is as low as $0.49 (500 pills) | 5/5 |
| Discounts | Bulk order discounts, Bitcoin payments (20%), returning customers ($25 off) | 5/5 |
| Customer Reviews | Great quality product for a low-price. I was very satisfied with the shipping speed and the customer service is truly unmatched. I have ordered from four different sites for Modafinil and this is by far the best service I have received. Thank you MXL! | 5/5 |
| Product Range | ModaXL, Modvigil, Modalert, ArmodaXL, Artvigil, Waklert, Modaheal, Vilafinil, Modafresh, sublingual Modafil MD | 5/5 |
| User Experience | The website is incredibly easy to navigate, and the payment portal includes Bitcoin, PayPal, eCheck, FastPay, and credit card payments (some users may experience declined transactions going from overseas). | 4/5 |
A) ModafinilXL: Price Point
ModafinilXL offers average pricing on their products. Both domestic and international shipping options are available for customers from the United States, Australia, the United Kingdom all European countries, including Denmark, Sweden, Norway, and Switzerland.
The cost per pill for modafinil is $0.49–$2.99.
For armodafinil, the cost ranges from $0.49–$2.99 as well.
The variability in price depends on the size of the order. You can get each product in quantities of 10, 20, 50, 100, 200, and 300. The more you buy at a time the cheaper the cost per pill becomes. Check out their bestselling Superio Combo Pack which may include any modafinil brands available in their store.
This is very standard pricing for the industry. Some companies sell it for a few cents more or a few cents less.
Where ordering from ModafinilXL makes up for this, however, is in discount options, and their shipping policy.
B) ModafinilXL: Discounts
ModafinilXL offers two generous discount options:
1. Returning Customer Discounts
The second discount they offer is aimed at returning customers.
All you need to do to apply it is to enter your returning customer discount at checkout to receive a $25 off your order.
This discount can’t be applied on top of Bitcoin discounts, so total savings can’t exceed 20%.
These discounts combined place their pricing well below the average for the industry.
2. Payment With Bitcoin (or Other Altcoins)
For those who don’t know, Bitcoin is a digital currency. It’s a store of value that uses advanced software programs to eliminate the need for central banks. People are using it more and more for purchases online and in-person as the technology develops.
ModafinilXL offers a 20% discount on the total order when paying with Bitcoin or other cryptocurrencies.
Currently, ModafinilXL Accepts 55+ Altcoins Including The Following Cryptocurrencies:
- Bitcoin (BTC)
- Ethereum (ETH)
- Litecoin (LTC)
- Dash (DASH)
- Ripple (XRP)
- Monero (XMR)
- Zcash (ZEC)
- DOGEcoin (DOGE)
- Ethereum Classic (ETC)
- Verge (XVG)
- NEMcoin (XEM)
Paying with cryptocurrency brings the price ranges down to $0.49–$1.94 for each modafinil tablet and $0.51–$1.99 for each armodafinil tablet.
Learn how to buy and use Bitcoin.
Total Price Differences With Discounts
(Prices based off orders of 300 tablets)
| Discount | Modalert | Modvigil | Waklert | Artvigil |
| None | $1.33 | $0.99 | $1.33 | $0.99 |
| Returning Customer ($25) | $1.25 | $0.91 | $1.25 | $0.91 |
| eCheck (10%) | $1.19 | $0.89 | $1.19 | $0.89 |
| Bitcoin (20%) | $0.86 | $0.65 | $0.86 | $0.65 |
Total Savings With Discounts
(Prices based off orders of 300 tablets)
| Discount | Modalert | Modvigil | Waklert | Artvigil |
| None | -$0.00 | -$0.00 | -$0.00 | -$0.00 |
| Returning Customer ($25) | -$25 | -$25 | -$25 | -$25 |
| eCheck (10%) | -$39.90 | -$29.90 | -$39.90 | -$29.90 |
| Bitcoin (20%) | -$139.65 | -$104.65 | -$139.65 | -$104.65 |
C) ModafinilXL: Customer Reviews
It’s hard to find a bad review about this company. Most of the complaints come from packages getting caught at the border. This problem is easily solved as ModafinilXL offers a delivery guarantee. They will reship the order exactly as it was.
Nobody can stop border security from looking inside a package, however, this is extremely uncommon, and there are things that can be done to minimize the chances of this happening.
It’s very rare for two packages to be stopped at the border twice in a row. The vast majority of orders end up at the customer’s door in a timely fashion.
D) ModafinilXL: Product Range
ModafinilXL offers the four main generic options of modafinil and armodafinil as well as the following generic brands Vilafinil, Modaheal, Modafresh, and sublingual Modafil MD. They don’t sell any other nootropics or other generic options (like Modawake or R-Modawake) at this moment.
Products offered by ModafinilXL:
| Modafinil or Armodafinil | Manufacturer | Link to Buy | |
| ModaXL (fastest onset effects) | Modafinil | HOF Pharmaceuticals | Buy Now |
| Modavinil | Modafinil | Centurion Remedies | Buy Now |
| Modalert | Modafinil | Sun Pharma | Buy Now |
| Modvigil (low-cost) | Modafinil | HAB Pharma | Buy Now |
| ArmodaXL (fastest onset effects) | Armodafinil | HOF Pharmaceuticals | Buy Now |
| Armodavinil | Armodafinil | Centurion Remedies | Buy Now |
| Waklert | Armodafinil | Sun Pharma | Buy Now |
| Artvigil (low-cost) | Armodafinil | HAB Pharma | Buy Now |
E) ModafinilXL: User Experience
The user experience on ModafinilXL’s website is logical and easy to navigate. Right on their homepage, they have a selector that includes all of the products they carry, with clearly marked pricing depending on the number of tablets ordered.
At checkout, they make it simple to select any coupon codes, discounts, and payment options — including credit cards (which isn’t commonly accepted for online pharmaceutical sales).
They’ve truly mastered the user experience in the modafinil space.
A Note on Shipping With ModafinilXL
One of the biggest advantages of ModafinilXL over other vendors is that they offer free international tracked shipping to most countries including the European Union.
Due to the stringent import regulations in some countries, ModafinilXL won’t ship directly to some countries. For these countries, a mail forwarding service will need to be used from a neighboring country to get the package to your doorstep. Alternatively, consider using Afinil.com if you live in Europe.
The countries ModafinilXL will not send to include:
| Austria | France | Mexico | Slovenia |
| Belgium | Germany | Monaco | South Africa |
| Brazil | Greece | Norway | Spain |
| Canada | Hungary | Pakistan | Sweden |
| China | Iceland | Poland | Taiwan |
| Croatia | Indonesia | Portugal | The Netherlands |
| Cyprus | Ireland | Romania | The Philippines |
| Czech Republic | Israel | Rwanda | The United Arab Emirates |
| Denmark | Italy | Saudi Arabia | |
| Estonia | Lithuania | Serbia | |
| Finland | Luxembourg | Slovakia |
As of January 2024, ModafinilXL resumed shipping to all EU countries from their warehouses located in Poland, Slovakia, France, and Germany.
The company is well aware of the issues involved with shipping modafinil overseas (albeit rare). In order to provide the best customer service experience possible for their customers, they guarantee delivery to your door.
If the first package doesn’t arrive, they’ll ship a second one free of charge. They also use a number of packaging and billing techniques to reduce the chances of inspection by border security officers.
The Pros & Cons of ModafinilXL
| Pros: | Cons: |
| Excellent customer service | Average pricing |
| Free tracked international shipping | Won’t ship directly to some countries |
| Accepts multiple forms of payments | |
| Guaranteed delivery | |
| Offers multiple discounts |
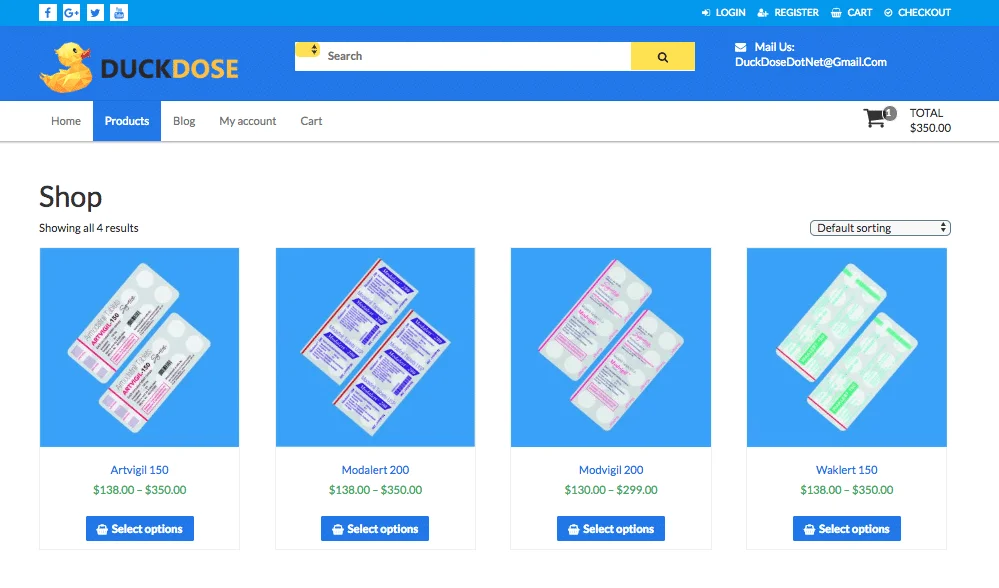
2. DuckDose
Update: DuckDose has recently shut down. ModafinilXL is now our number one recommended source for buying modafinil online.
The online modafinil vendor DuckDose is a leader in the international modafinil market.
They were one of the first companies on the scene to start selling discounted generic Provigil tablets online.
Prior to the introduction of DuckDose, anybody looking to buy modafinil needed to either have a prescription for it — and pay full price for brand name Provigil — or source it on the black market. Buying modafinil on the street is extremely dangerous and not recommended. Many dealers are selling dangerous and addictive drugs as modafinil to get their customers hooked.
DuckDose stepped in, offering legit pharmaceutical grade, lab-certified modafinil online without the need for a prescription.
DuckDose Review Summary
| Overall Rating | Details | 4/5 |
| Price Point | Average pricing. Modafinil cost is as low as $0.70 while Armodafinil cost is as low as $0.90 | 4/5 |
| Discounts | Bulk order discounts only | 2/5 |
| Customer Reviews | Excellent product; really helps give me an extra boost when working two jobs. It helps my mood and overall well being. | 5/5 |
| Product Range | Modvigil, Modalert, Artvigil, Waklert | 4/5 |
| User Experience | User experience ahead of its time 10 years ago, but slightly outdated now. Payment portal only accepts Bitcoin. | 3/5 |
How Does DuckDose Work?
How can DuckDose sell prescription modafinil without a prescription legally?
It’s simple…
DuckDose, and most other modafinil vendors that followed distribute their modafinil from India, where it’s fully legal to sell modafinil without the need for a prescription. It’s also the home of the two major generic modafinil vendors — HAB Pharma and Sun Pharma.
Sending modafinil orders from India makes the operation fully legal. The worst that will happen is your order will be flagged at the border, pending the submission of a prescription. If you don’t have a prescription, all you have to do is contact customer service at DuckDose and they’ll send you an identical order.
DuckDose is well-loved by the modafinil community and is considered to be one of the best vendors in this space.
A) DuckDose: Customer Service
DuckDose is known for their customer service. They are thought to have set the tone for most of the industry. Their moderators are frequently responding to comments and discussions in their online forum, and are fast to respond to any issues.
B) DuckDose: Price/Value
DuckDose offers average pricing on its modafinil products. Bulk discounts are available for larger orders.
C) DuckDose: Discounts
Unlike many of the other vendors in this space, DuckDose doesn’t offer any discounts above and beyond their bulk order discounts.
D) DuckDose: Customer Reviews
This is an area where DuckDose stands out above the pack. They have an entire subreddit dedicated to their customer fan base. People love the quirky nature of the website, covered in ducks and vibrant colors. It has character as a vendor, excellent products, top-notch customer service, and an innovative forum dedicated to delivering high-value advice and information to their customers.
E) DuckDose: Product Range
DuckDose offers the standard generic modafinil products:
- Modalert
- Modvigil
- Waklert
- Artvigil
F) DuckDose: User Experience
The user experience with DuckDose is acceptable but could use some upgrades. Some of the pages feature small text, and it appears to be made with older generations of CSS and HTML.
Their payment portal is easy to navigate but doesn’t accept credit cards at this time.
The Pros & Cons of DuckDose
| Pros: | Cons: |
| The website is not as user-friendly as other options | Update: No longer in business |
| Veterans in the modafinil space | Price is more expensive than newer websites |
| Large online educational forum | |
| Multiple generic options of modafinil | |
3. ModUp
Update: ModUp has recently shut down. ModafinilXL is now our number one recommended source for buying modafinil online.
ModUp is best known for its customer service excellence.
They respond to customer emails or support tickets within about a day and are extremely helpful. This is a stark contrast to the average modafinil vendor in this space, which can take weeks to get a suitable answer to a question or issue.
ModUp also has a large, thriving community found on their online forums. Here, modafinil users and nootropics aficionados have the opportunity to share information and talk about all things modafinil.
This is a great resource for information on modafinil and other nootropics among new and experienced users alike.
ModUp Review Summary
| Overall Rating | Details | 3/5 |
| Price Point | Average pricing on Modalert even with a generous discount | 3/5 |
| Discounts | Bulk order discounts and a 23% Bitcoin discount | 5/5 |
| Customer Reviews | This vendor has excellent reviews, but there are a few people upset at the poor product selection and slow delivery times | 3/5 |
| Product Range | Only Modalert | 2/5 |
| User Experience | Aside from the website being spammy with popups and ads, it’s easy to navigate and the payment portal is fast and secure. No credit cards accepted | 4/5 |
A) ModUp: Customer Service
ModUp has excellent customer service. All three of the vendors discussed in this article stand out here, but it’s important to consider how these are exceptions to the industry as a whole.
The biggest complaint online about various modafinil vendors is their terrible standard for customer service. Emails and complaints go unanswered, order confirmations or promised tracking information don’t arrive, and orders often either never show up, or appear 3 months after the promised delivery date.
ModUp is a leader in customer service for the modafinil industry, with lighting fast response times, and knowledgeable staff on the other end.
Two thumbs up for ModUp customer service reps.
B) ModUp: Price/Value
ModUp isn’t known for its pricing.
They only sell one product and have a generous 23% Bitcoin discount (more on this below). Despite this, their products are still about the average price compared to other vendors, if not slightly above average.
They also charge for shipping, adding extra fees at the time of checkout.
C) ModUp: Discounts
ModUp offers the best Bitcoin payment discount I’ve seen yet. They offer a whopping 23% for anybody paying with Bitcoin! That’s well above and beyond the industry norm, however, their higher prices and cost of shipping level this discount out.
You can expect to pay about the average going rate for Modalert when buying from ModUp.
D) ModUp: Customer Reviews
In general, ModUp has excellent customer reviews. People are impressed with their fast delivery and email response times.
There are, however, some negative reviews, with people attacking their small product range (only one product), and some people complaining about slow delivery times. We have the impression that those experiencing slow delivery times may be experiencing this due to border security more than the company itself. This is because there are a lot more reviews raving about how fast they received the order in the mail after ordering it.
Generally, you can expect to receive your package in about 7–15 days after ordering from ModUp.
E) ModUp: Product Range
One of the biggest cons of ModUp is that they only have one product for sale — Modalert.
This isn’t a deal-breaker for us, because Modalert is an excellent generic product, and offers virtually identical effects to the brand name options like Provigil. However, there are some subtle differences between all the generic options currently on the market. There is an even bigger difference between Modalert and armodafinil products like Artvigil and Waklert.
Without the option to test these other forms out, ModUp’s customer base can’t dial in their modafinil as closely as they can from ordering from other websites that sell all of these products.
Modafinil reacts differently in everyone, so testing different products out to find what works best for the individual is recommended. In order to do this, you’ll need to use other vendors as well as ModUp.
This is my biggest complaint about ModUp.
F) ModUp: User Experience
ModUp gets 4/5 for user experience. Their website is easy to use, but I find it a bit too spammy. There are ads, and lots of pop-ups interrupting my flow. I also have to find the products on separate pages, which is simple but includes additional steps compared to their competition like Afinil Express and DuckDose.
The Pros & Cons of ModUp
| Pros: | Cons: |
| Offers the best discount options (23%) | Update: ModUp is no longer in business |
| Excellent customer service | They only carry one product (Modalert) |
| Hosts a thriving online forum | They charge for shipping and don’t ship to all countries |
Our Personal Favorite
Updated
Due to the closing of Afinil Express, ModUp, BuyModa, and DuckDose in 2019-2023, we’ve focused our attention primarily on ModafinilXL as the best modafinil vendor. All three were excellent options, however, times change and the modafinil space is rapidly evolving. Many of the best vendors of the past are starting to disappear.
Compared to newer vendors we still prefer ModafinilXL because of their large and loyal customer base, the establishment in the modafinil space, and excellent discount options.
They offer all four of the most common generic modafinil versions – ModaXL, Modavinil, Modalert, Modvigil, ArmodaXL, Waklert, and Artvigil. Check out their bestselling Superior Combo Pack which may include any modafinil brands available in their store.
Updated : Modalert & Waklert are currently not available for sale worldwide. The manufacturer has limited the export of these modafinil generics abroad, now Modalert 200 mg and Waklert 150 mg can be purchased if you live in India. Therefore, we suggest considering excellent alternatives with the purest formula and excellent quality overall – ModaXL 200mg & ArmodaXL 150mg by HOF Pharmaceuticals. You can order nootropics from reliable suppliers all over the world!
With free tracked international shipping, it’s easy to follow your order all the way to your doorstep. If there are any problems, they’ll either provide a full refund or reship an identical order until it makes it through the border.
These are all great customer service traits, and we’ll continue to use them for our own modafinil supply for the immediate future.
This post is also available in:
Français
Deutsch
Italiano
Русский
Español